Magnetic Resonance Imaging in Gynecology
Authors
INTRODUCTION
Magnetic resonance imaging (MRI) is an imaging modality that has been developed and used since the mid-1970s. MRI has several advantages over computed tomography (CT) and ultrasonography. One important feature is its noninvasiveness. The imaging components include a large static magnetic field and an electromagnetic field produced by radio frequency (RF) waves. Although once termed nuclear magnetic resonance imaging, MRI uses no ionizing radiation. The nucleus being studied in this form of imaging is the naturally occurring hydrogen nucleus, a proton, which is ubiquitous in the body by virtue of its presence in water.
A second feature that makes MRI particularly attractive is its capability for multiplanar imaging. Without repositioning the patient, transverse, sagittal, coronal, and nonorthogonal views may be obtained in a short time. Such capabilities allow excellent study of normal and abnormal anatomy. Compared with MRI, ultrasonographic examination allows more tissue planes to be observed in real time. However, the window of view is actually relatively small, and a simultaneous display of a large portion of the body is not possible.
A third advantage of MRI is its excellent tissue-differentiating capabilities, made possible because the biochemical characteristics of the nuclei within their microscopic environment alter the information (called signals) received during an MRI acquisition. MRI acquisitions may further alter and differ contrast. These signals are not influenced by the amount of bladder filling, the size of a patient, or the amount of gas in the surrounding bowel, but these factors have an important role in the quality of an ultrasonographic image. With MRI, excellent tissue differentiation is possible without the use of contrast agents. However, newly developed contrast agents may further augment tissue contrast and are much safer than the iodinated equivalents used in CT.
A fourth advantage of MRI is its intrinsic sensitivity to flowing blood. As with Doppler ultrasonography, flow direction and speed may be determined. Both arterial and venous abnormalities can be assessed by MRI. Additionally, biochemical states of blood can be characterized by MRI because characteristic signals are derived from oxyhemoglobin, deoxyhemoglobin, methemoglobin, and hemosiderin in red blood cells in different stages of hematoma formation. Together, these two capabilities for studying blood allow sensitive MRI diagnosis of thrombotic diseases.
Ultrasonography and CT scanning are now the primary imaging modalities used in gynecology. However, it is clear that MRI can serve as an alternative or an adjunctive tool in many instances. In this chapter, we discuss the basic principles of MRI, the utility of this tool for recognizing normal pelvic anatomy, and the current role of MRI in studying pelvic pathology.
NUCLEAR MAGNETIC RESONANCE PRINCIPLES IN IMAGING
Nuclear Spin
Certain atomic nuclei in molecules possess nuclear angular momentum, or spin. Such nuclei may be considered as spinning charged particles that create a magnetic field or moment (μ). 1H, 31P, 13C, 15N, and 19F are nuclei with spins. 1H nucleus, the proton, is currently the only nucleus extensively used for MRI because of its relative abundance in the human body; therefore, it will be the focus of the remainder of this discussion.
In the absence of an external magnetic field, individual hydrogen nuclei are randomly oriented within a tissue. When a uniform external magnetic field (B0) is applied to these nuclei, the nuclei tend to align in the direction of the applied field because this is the lowest energy state. The aligned nuclei will spin, or precess, about E0 at a frequency that is determined by the strength of the magnetic field being sensed by the nuclei—that is, the larger the external magnetic field, the higher the frequency of precession. The magnetic moments of multiple similarly aligned nuclei produce a net magnetic moment that is used to produce the MRI signal (Fig. 1A).
Alignment in a direction opposite to the external magnetic field requires nuclei to be in a higher energy state. The quantity of energy required to transform the proton to its higher energy state is determined by quantum mechanical principles and is directly related to the precession frequency of the proton.
Such transfer of energy may be achieved by applying an electromagnetic field (B1) (which for imaging is in the range of RF wavelengths) orthogonal to the main magnetic field (B0). The net magnetic moment vector will rotate about the original magnetic field, the degree of rotation being determined by the strength and duration of the applied electromagnetic field. Assuming E0 to be oriented in the Z direction, then the net magnetic moment is usually rotated 90°, thus placing the net magnetic moment vector into the X-Y plane perpendicular to the direction of E0 (Fig. 1B). When the electromagnetic field is discontinued, the net magnetic moment vector precesses in the X-Y plane. This precession of the net magnetic moment vector is also known as transverse magnetization.
This precession in the transverse plane, the X-Y plane, will induce a voltage within coils or loops of wire that are aligned with the transverse plane. This induced voltage is then translated into a signal that results in a magnetic resonance image. It is the ability of MRI to assess variations in the net magnetization of the nuclei within different tissues that allows for superb tissue contrast, a unique feature. These variations in net magnetization decrease exponentially over time and are characterized by T1 and T2 relaxation times that are unique to the specific tissue. These relaxation times are explained in the paragraphs that follow.
T1 Relaxation
After electromagnetic excitation, nuclei absorb energy and a higher percentage of the nuclear population exists at a higher energy state. By transferring this energy from the excited nuclei to surrounding molecules, commonly referred to as the lattice, the nuclei return to a lower energy state, realigning with the main magnetic field (B0). This return to the low energy state is called T1 relaxation or spin lattice relaxation. The efficiency with which energy is transferred depends on the molecular structure of the surrounding tissues (i.e., relaxation of protons in fat would differ from relaxation of protons in muscle). The transfer of energy is described by an increasing exponential function in which the time constant (i.e., the time at which 63.7% of the previously displaced spins realign with the main magnetic field) is the T1 relaxation time. Shorter T1 relaxation times imply faster realignment with the main magnetic field after excitation.
T2 Relaxation
After excitation, the nuclei initially precess coherently within the X-Y plane. However, as a result of local fluctuations in the magnetic field caused by nearby nuclei, energy is transferred from one nucleus to another. This transfer of energy results in loss of phase coherence. Macroscopically, the net magnetic moment vector decreases, resulting in a smaller signal. T2 relaxation describes this loss of phase coherence or transverse magnetization. It is also known as spin-spin relaxation, because energy is transferred from one excited spin (nucleus) to another and not to the lattice as in T1 relaxation. This transfer of energy is characterized by an exponential decay function in which T2 relaxation is the time necessary to lose 63.7% of the signal. T2 relaxation typically occurs more rapidly than T1 relaxation and is the primary cause of the exponential decay in transverse magnetization.
Spin-Echo Imaging
Because of imperfections in the main magnetic field, nuclei lose their phase coherence (i.e., their ability to precess in synchrony with surrounding nuclei), and transverse magnetization decreases more rapidly than anticipated based on known T2 relaxation values of a sample tissue. It can be shown that a 180° RF pulse applied at some time after the 90° RF excitation can re-establish phase coherence. The time phase coherence that is re-established is called the echo time (TE), and the use of a 90° excitation pulse followed by a 180° RF pulse is known as a spin-echo sequence (SE). The signal generated from such a sequence approximates the signal anticipated based on the tissue T2 relaxation times (Fig. 2).
To produce an image with a resolution of 128 by 128 pixels, the entire procedure for excitation and signal acquisition must be repeated at least 128 times. For typical areas imaged in the pelvis, this technique yields resolution in the range of 1 mm to 4 mm. In spin-echo imaging, the time from the application of the first 90° RF pulse to the application of the next 90° pulse is called the repetition time (TR).
Spatial Localization
To produce a magnetic resonance image, a signal must be generated and localized. The scientific breakthrough that finally allowed creation of an image using the principles discussed earlier followed the discovery that signal localization is possible with use of superimposed linear electromagnetic fields, or gradients, on B0. In the presence of such gradients, nuclei in the weaker part of the field will precess more slowly than those in the stronger parts of the field, thus allowing localization of each individual signal.
Tissue Contrast
By adjusting the TR and TE intervals, it is possible to make either T1 or T2 contrast more prominent within an image. Short TR and TE combinations (commonly written TR/TE-e.g., 500/20 msec) accentuate T1 contrast, whereas long TR and TE combinations (e.g., 2500/80 msec) preferentially select for contrast based on differences in T2 relaxation. Accordingly, short TR/TE images are considered T1 weighted and long TR/TE images are considered more T2 weighted.
The appearance of an image changes markedly depending on the emphasis of T1 or T2 relaxation times. For example, on a T1-weighted image, fat appears bright (white), whereas fluid appears dark. On a more T2-weighted image, fat appears gray, whereas fluid appears bright (white). Most but not all pathology, because of its increased water content, mimics fluid—that is, it is dark on T1-weighted images and bright on T2-weighted images (Table 1).
TABLE 1. Magnetic Resonance Signal Intensity of Tissue
Tissue | T1-Weighted Images | T2-Weighted Images |
Fat | Increased | Slightly increased |
Blood | Variably increased | Variably increased |
| or decreased | or decreased |
Pus | Slightly decreased | Increased |
Inflammation | Decreased | Increased |
Edema | Decreased | Increased |
Serous fluid | Decreased | Increased |
Other Pulse Sequences
Nuclei may be excited in ways that differ from the spin-echo technique described earlier. Such different excitation techniques are called pulse sequences. Depending on the particular sequence, contrast mechanisms may be significantly altered. Although spin-echo imaging is currently the single most common type of imaging sequence used, several new pulse sequences are increasingly being adopted.
Applying a 180° RF pulse before the 90° sequence of a spin-echo technique creates an inversion recovery pulse sequence. Appropriate timing of the distance between the first 180° and the 90° pulse allows for the creation of an image in which final contrast depends on both T1 and T2 relaxation differences. This technique may potentially be more sensitive to subtle pathologic changes than conventional spin-echo imaging.
One of the inherent disadvantages of conventional MRI is the long acquisition time (range of 1–20 minutes for 9–40 images). Gradient recalled echo sequence is a whole family of pulse sequences known by acronyms such as FLASH, GRASS, and FISP; they produce images in as little as 3 to 5 seconds. Such techniques differ from standard spin-echo imaging by using gradients to generate the signal, foregoing the 180° RF pulse and initially exciting the protons at some angle that typically is not 90°. Contrast developed by these techniques depends not only on the TR and TE but on the angle of excitation (flip angle) as well. An added advantage of these techniques is that flowing blood registers a consistently high signal. Their precise clinical utility is currently undergoing intensive evaluation.
Recently, a new class of sequences known by acronyms such as RARE, Fast Spin Echo, and Turbo Spin Echo have become clinically available. These sequences are capable of producing T2-weighted images with contrast similar to that of conventional spin-echo imaging in one half to one quarter of the acquisition time. These imaging techniques are expected to replace conventional T2-weighted spin-echo imaging of the pelvis over the next several years.1, 2, 3, 4
INSTRUMENTATION
MRI instrumentation typically consists of the horizontal superconducting magnet with RF gradient coils embedded within it, a sliding bed that moves the patient into the magnet, a computer for image reconstruction, a display system, and an image printer. Imaging is now performed with magnets having field strengths ranging from 0.08 tesla (T) to 2 tesla (10,000 gauss [G] = 1 T). The average cost of an MRI system varies between$1 million and $2 million. The average time for a traditional MRI gynecologic examination is approximately 1 hour. However, with the advent of phased array surface coils and fast spin-echo sequences, this time is rapidly decreasing. At our institution, the costs of an MRI gynecologic scan and a CT scan are approximately equivalent.
SAFETY
Although the large static and oscillating magnetic fields used in MRI may pose some theoretic adverse biologic risks, no ill effects have been demonstrated with exposure levels currently used in imaging. Long-term exposure to the large static magnetic fields has been studied in workers who were exposed to magnetic fields of up to 2 T in their occupation. No long-term ill effects have been noted.5
The rapidly changing electromagnetic fields from the gradient coils surrounding the patient have been evaluated for potential induction of electric currents within tissue. The gradients used in imaging are less than those necessary to induce cardiac arrhythmias.5 Heat deposition is another potential concern, but body temperature probes have failed to demonstrate temperature elevations. Large metallic prostheses, such as those in limbs, may, theoretically, absorb significant amounts of RF emissions and result in local heating. However, such patients have been imaged on a routine basis, and adverse heating effects have not been noted.
MRI in patients with cardiac pacemakers is absolutely contraindicated because of magnetic field effects on the device. Most pacemakers are operated by switches that are magnetically controlled. Another potential risk is injury from flying metal objects that are drawn to the magnet. Accordingly, patients entering the MRI unit should be wearing no metallic objects (e.g., hairpins, pens). Patients with surgical ferrous intracranial aneurysm clips and embedded shrapnel are also excluded from MRI. Surgical clips and most other surgical hardware are acceptable by about 6 weeks after surgery, although safety considerations may require evaluation on a case-by-case basis.
Finally, one significant concern is claustrophobia, because patients lie on a sliding bed that is then placed within the magnet, which is approximately 52 cm in diameter and 6 feet long. Approximately 1% to 5% of patients are mildly uncomfortable. Appropriate patient support or medication may be necessary to complete the requested study.
GYNECOLOGIC IMAGING
Normal Pelvic Anatomy
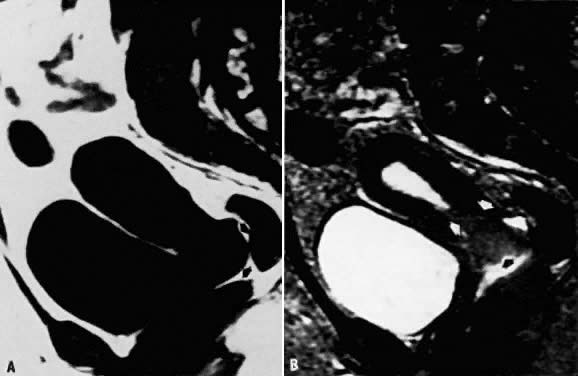
The applicability of MRI in the female pelvis has been intensively evaluated since the early 1980s. Normal female pelvic anatomy is well depicted (Fig. 3).6 On T1-weighted images, the uterus is easily identifiable and appears as a homogeneous structure of medium signal intensity with indistinct internal architecture. However, on T2-weighted sequences, the corpus, isthmus, and cervix are distinguishable. The myometrium of the fundus is intermediate in signal intensity, whereas endometrium appears as high signal intensity. The two regions are separated by a junctional zone of low signal intensity. Although there is some debate in the literature, this zone is believed to represent myometrium, and the signal difference is due to decreased water content.7 The zonal structure within the uterus is markedly influenced by hormones. Women in the follicular phase of the menstrual cycle demonstrate a thin endometrium. However, the endometrium increases in thickness through the menstrual cycle and is most prominent in the midsecretory phase. On T2-weighted images, the signal intensity of the myometrium is higher during the secretory phase than during the proliferative phase. The total uterine volume also increases and is greatest during the secretory phase. Women who are on oral contraceptives demonstrate a markedly different uterine appearance. In these women there is no clear distinction between the myometrium and the endometrium, and the endometrial tissue appears to be thin and atrophic. Premenarchal and postmenopausal uteri appear similar, demonstrating both thin endometrium and small uterine volume.
The cervix is easily visualized on MRI, and the length and orientation are easily determined with T2 weighting. The normal cervix has two separate zones, a central zone of high signal intensity representing the endocervical canal containing mucus, and an outer zone of cervical stroma that demonstrates low signal intensity. On T1-weighted images, the parametrium surrounding the cervix is imaged as medium signal intensity and is easily distinguished from the low-intensity cervical stroma.
The vagina can be distinguished from the surrounding structures on T2-weighted images. It also has a high-intensity center representing mucus in the vagina and varies in thickness, being thinner in the follicular phase of the menstrual cycle in normal menstruating females, in premenarchal girls, and in postmenopausal women not on estrogen replacement. The wall of the vagina itself is of low signal intensity on T2-weighted images in the early follicular phase of the menstrual cycle but increases to medium intensity in the secretory phase.8 Transverse images allow easy identification of the vagina, whereas sagittal images allow clear distinction between the posterior vaginal fornix and the cervix and rectum.
Normal ovaries tend to have low to medium signal intensity on T1-weighted images. On T2-weighted images, the signal intensity increases and approaches that of surrounding fat (Fig. 3 C, D). Large follicular cysts may have greater signal intensity than fat, making it easier to identify the ovaries using this pulse sequence, but there may be some difficulty in distinguishing them from surrounding bowel loops. Ovaries are more difficult to distinguish and inconsistently visualized in postmenopausal women.9
By MRI, the pelvic musculature is easily identified and is lower in signal intensity compared with fat. The vesicovaginal septum, the rectovaginal septum, and the levator ani muscle can be identified.10 The urethra is also easily demarcated, and its relationship to the bladder can be studied. The bladder is identified without any difficulty. The bony pelvis is also easy to visualize, and some investigators have used MRI for obstetric pelvimetry, the advantage being that it uses no ionizing radiation.11 Because there is little “free” water in cortical or trabecular bone, the signals originate from the marrow within the bone rather than from the bone itself.
SPECIFIC GYNECOLOGIC PATHOLOGY
Uterus
Normal myometrium in women not on oral contraceptives demonstrates an increase in T1 and T2 relaxation times in the secretory phase of the menstrual cycle. On more T2-weighted images, an increase in signal intensity is evident. The appearance of the myometrium in women on oral contraceptives is one of higher signal intensity on T2-weighted images, whereas the endometrial tissue is markedly reduced.12 Women taking higher doses of oral contraceptives demonstrate a larger degree of myometrial swelling and endometrial atrophy. It is thought that there is a greater water content in the myometrium during the mid-secretory phase and that there is an increase in the T1 and T2 relaxation times, resulting in increased signal intensity on T2-weighted images and decreased intensity on T1-weighted images.
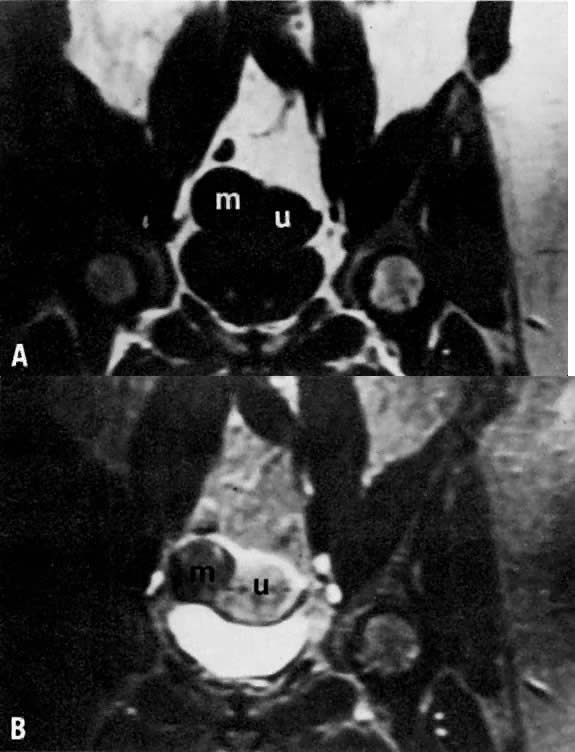
Knowing the normal myometrial characteristics of the uterus allows identification of pathologic alterations such as leiomyomas, a common gynecologic disorder (Fig. 4). Simple myomas tend to be of low signal intensity regardless of the pulse sequence used.13 They are usually surrounded by a smooth capsule also of low signal intensity. When compared with ultrasonography or hysterosalpingography, MRI is more accurate in detecting the presence, size, number, and location of leiomyomas.14 In patients with menorrhagia or infertility secondary to submucosal leiomyomas, MRI may be useful in optimizing patient management. In patients undergoing myomectomies to restore fertility, MRI before the procedure may help in planning the extent of surgery.
Leiomyomas have various appearances depending on the presence or absence of calcium, hyaline or cystic degeneration, and hemorrhage.15 In the presence of cystic degeneration, the leiomyoma demonstrates increased T1 and T2 relaxation times, whereas the degenerative area itself has low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Hemorrhage within the leiomyoma, however, produces various appearances, depending on the imaging sequence used, and can make the diagnosis of leiomyoma more difficult.16
Several investigators have explored MRI of uterine sarcomas. Although MRI demonstrates the presence of these massive lesions and the degree of myometrial invasion, the overall findings are nonspecific, and differentiation from endometrial carcinoma is difficult.17, 18
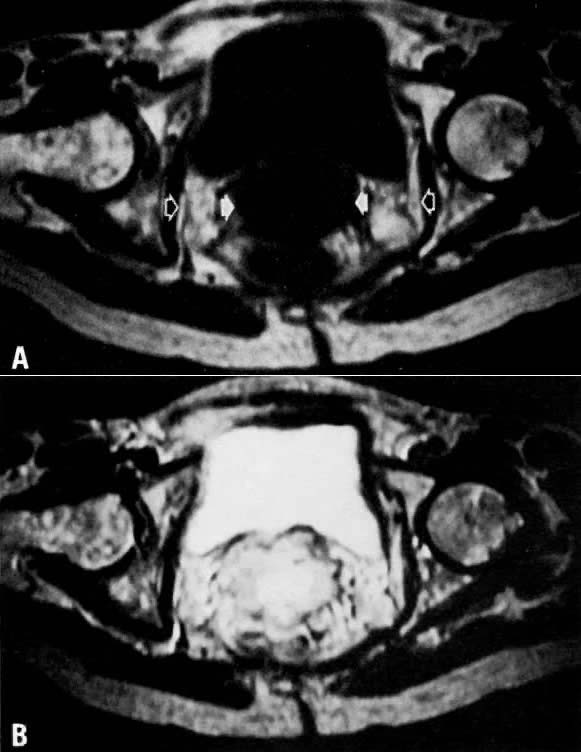
Adenomyosis is a relatively common condition occurring in approximately 15% to 25% of women in the premenopausal period. It leads to progressively heavier and longer menstrual periods and is often associated with severe dysmenorrhea. The diagnosis is typically made after hysterectomy from pathologic specimens. MRI has been used to evaluate this condition.19, 20 On imaging, uteri with adenomyosis are enlarged and have smooth external configurations. Diffuse adenomyosis distorts the normal zonal anatomy of the uterus, causing enlargement of the junctional zone (Fig. 5). Although predominantly isointense with myometrium on T1-weighted images and decreased in signal on T2-weighted images, old hemorrhagic areas measuring a few millimeters in diameter are often seen as high-intensity spots on both T1-weighted and T2-weighted images. In contrast to leiomyomas, which have well-circumscribed margins, adenomyosis has irregular and indistinct margins because of its more invasive nature. Mark and colleagues reported on 21 patients with suspected adenomyosis.20 MRI correctly diagnosed all eight cases of adenomyosis subsequently confirmed by pathology. In a series of 93 patients with uterine enlargement, Togashi and associates used MRI to correctly diagnose the 71 cases of leiomyomas, 15 of 16 cases of adenomyosis, and all 6 cases of simultaneous involvement of both conditions.21 Because adenomyosis is often treated by hysterectomy but myomectomy may be sufficient for some leiomyomas, such imaging may be a very useful clinical tool for preoperative assessment and surgical planning.
Endometrium
MRI is particularly useful for assessing the endometrium, which can easily be identified and distinguished from the myometrium. Experience to date demonstrates that the endometrial tissue is approximately isointense with myometrium onT1-weighted images but appears higher in signal intensity relative to myometrium on T2-weighted images. The thickness of the endometrium in a normal menstruating female varies depending on the phase of the menstrual cycle, being thinner in the follicular phase and thicker in the secretory phase.22 Among patients who use oral contraceptives, the endometrial width is significantly smaller in both the follicular and secretory phases. Additionally, the junctional zone is also smaller in both phases of the menstrual cycle. Myometrial thickness tends to remain the same regardless of the phase of the menstrual cycle and the use of oral contraceptives. Such differentiation allows better assessment of the endometrium and may be particularly useful when Asherman's syndrome is suspected. The normal endometrial width varies between individuals, ranging from 1 to 8 mm, whereas the myometrial width varies from 1.5 to 2.5 cm. During the normal follicular phase, endometrial width can grow from 1 to 3 mm.22
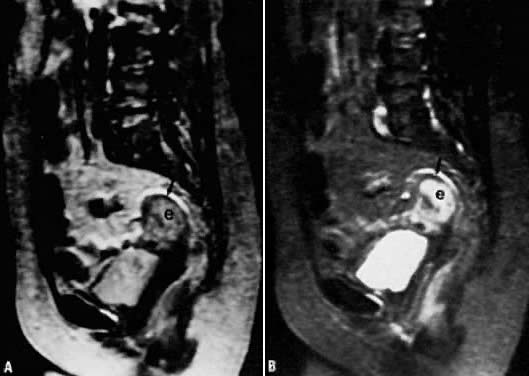
MRI is able to define depth of myometrial invasion, tumor site, and cervical involvement in patients with endometrial cancer.23 Invasion of the myometrium is demonstrated by distortion of the junctional zone (Fig. 6). In patients with deep myometrial invasion, this low-intensity band is absent. MRI allows preoperative evaluation of the degree of invasion before a postoperative pathology assessment. Although MRI cannot diagnose endometrial cancer in situ (confined to endometrium), it is 92% accurate in the overall staging of endometrial carcinoma.24 The overall accuracy in demonstrating depth of myometrial invasion ranges from 71% to 86%.24, 25, 26, 27, 28, 29 Cervical involvement has been evaluated by Powell and colleagues, who correctly detected cervical involvement in 11 of 12 patients.29 In the 12th patient there was only microscopic evidence of cervical invasion, which was below the resolution of MRI. Tumor volume, which can also be assessed by MRI, may be a more useful prognostic indicator than depth of myometrial invasion.
Gadolinium enhancement with dynamic imaging has recently been investigated with promising preliminary results. Because normal myometrium shows more enhancement relative to tumor, Hirano and colleagues were able to increase their sensitivity for detecting deep myometrial invasion from 89% to 91%.27 Yamashita reported an increased accuracy of 85% with dynamic imaging compared with 68% when relying on T2-weighted spin-echo images.28 This enhancement occurred 120 seconds after administration of the gadolinium-enhancing agent. With further investigations in this technique, diagnosis and evaluation of endometrial carcinoma will be improved.
Cervix
A normal cervix has two distinguishable zones on MRI. The stroma is of low signal intensity on T2-weighted images, whereas the endocervical canal is represented by high signal intensity. The multiplanar capabilities of MRI allow excellent visualization of the cervix and the surrounding tissue, which is sometimes difficult on CT or ultrasonographic examination.
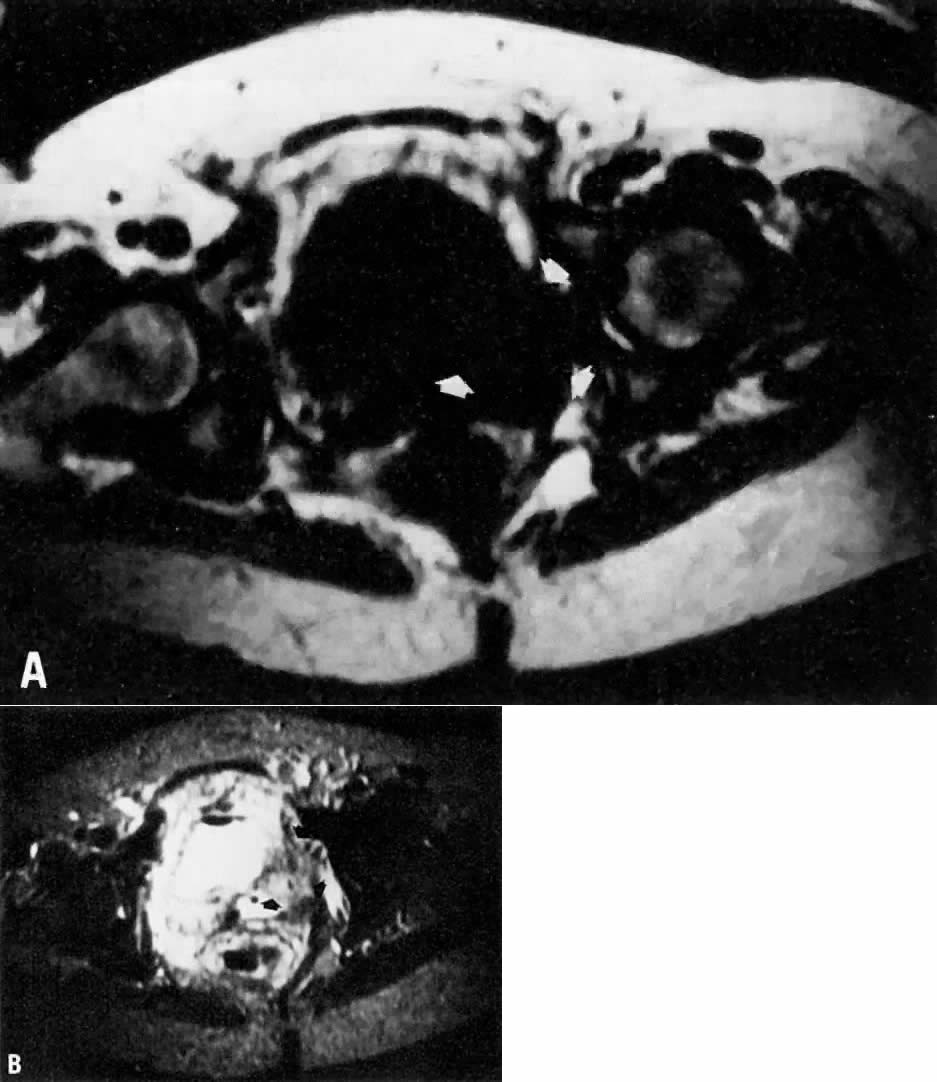
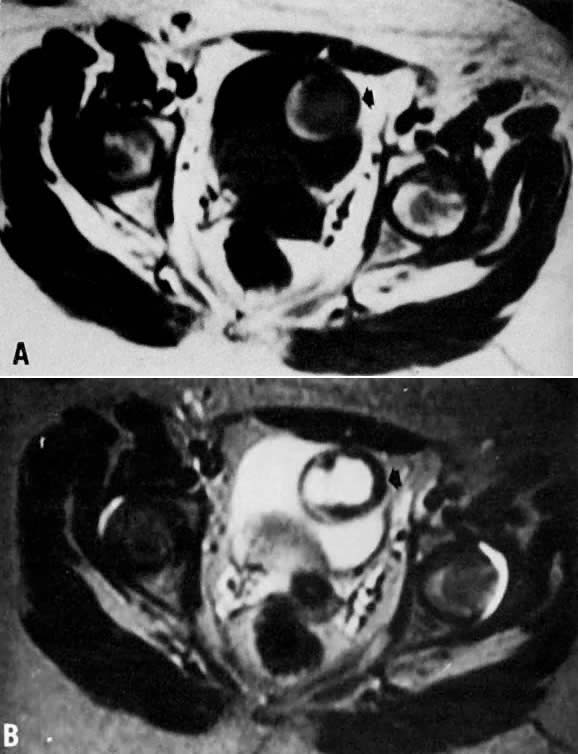
Cervical cancer has an overall poor survival in the presence of advanced invasive disease. Clinical staging has emphasized differentiation between Stages IB, IIA, and IIB. The distinction is important, because carcinomas staged less than or equal to IIA (i.e., disease without parametrial involvement) are usually treated with surgery, whereas carcinomas of Stage IIB or greater (i.e., disease with parametrial involvement) are usually treated with radiotherapy. Clinical staging of cervical cancer is currently performed by physical examination, chest radiography, cystoscopy, intravenous pyelography, and sigmoidoscopy. CT, the traditional method of radiologic staging, is limited by an inability to image in multiple planes and by poor soft-tissue delineation. MRI can detect cervical cancer, which has increased signal intensity on T2-weighted images in contrast to surrounding tissues; therefore, it is an important tool for clinical staging (Fig. 7).29
Although MRI detection of parametrial involvement should, in theory, be excellent, no rigid criteria are currently available (Fig. 8). Some authors have found MRI assessment of the parametrium to be 89% to 93% accurate.30, 31, 32 Others, however, have reported a slightly less impressive result of 79%.33 Some of the limiting factors may be distortion from hemorrhage and edema, as well as distention of the vaginal fornix by large lesions.32 Inflamed parametrial tissues secondary to ulceration and infection of the primary tumor or uterine instrumentation may affect the appearance of parametrial tumor involvement. Overall, however, experience thus far supports the greater accuracy of MRI in parametrial assessment compared with CT scanning. In 22 women imaged with both CT and MRI before surgery, MRI demonstrated an 86% accuracy rate in predicting the presence or absence of parametrial involvement, compared with 77% for CT.34 In another study, MRI was able to identify all six cases of parametrial extension, whereas CT detected only one case.35
MRI distinction of Stage IB from IIA is also reliable. Janus and colleagues report a 91% accuracy of MRI for detecting vaginal extension, compared with 77% for CT.34 Others have reported an accuracy rate of greater than 80%.32 Such assessment may be altered by distortion of the vaginal fornix as a result of the size of the lesion. In such cases, tumor volume, which can be accurately determined by MRI, may be an important parameter for determining prognostic factors.36
Compared with examination under anesthesia, MRI staging is superior. In one study, clinical examination under anesthesia underestimated the size and extent of the tumor in six of ten cases of Stage IB cancer patients.37 In contrast, MRI correctly staged nine of these ten cancers.
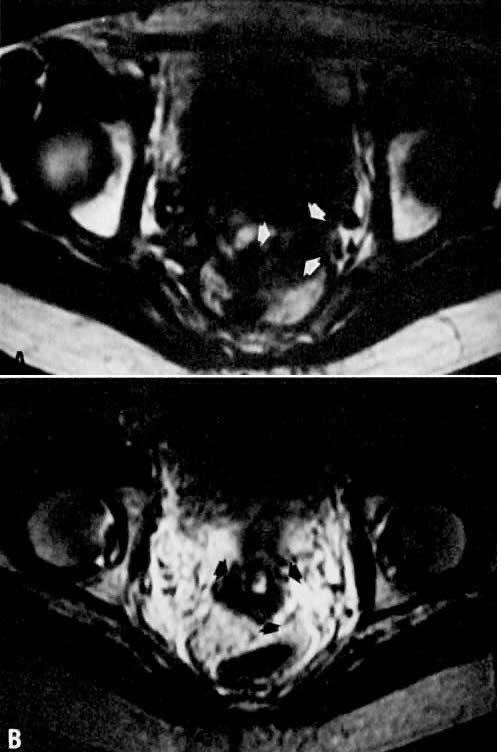
Recurrent cervical tumor can be distinguished from fibrosis by MRI. This capability is particularly exciting. The distinction between these two pathologies was reported by Ebner and colleagues, who noted that in all six patients with recurrent tumor, signal intensity in the tumor increased as the T2 weighting increased.38 This behavior was in contrast to that seen in fibrosis, which showed decreased signal intensity when the T2 weighting increased. Other investigators have confirmed these findings (Fig. 9 and Fig. 10).23, 39 It is important to note that the characteristics of fibrosis change with time—that is, early radiation-induced fibrosis produces high signal intensities on T2-weighted images, whereas older fibrosis yields low-intensity signals on the same scans. Overall accuracy of MRI in the diagnosis of recurrent tumor is 78%, with higher rates of accuracy and specificity after 6 months.40 CT scanning cannot distinguish between recurrent tumor and fibrosis in this manner. With ongoing development of paramagnetic contrast agents (substances that accumulate in tissue and shorten relaxation times), the diagnostic potential of MRI could be further extended.
An additional utility of MRI in cervical cancer has been its ability to assess and follow tumor volume and change in T1 relaxation times during and following therapy. Hawnaur and associates were able to demonstrate reduction in tumor volume.41 However, there was no demonstrable relationship between rate of tumor regression and prognosis. A better utility of MRI may derive from T1 relaxation times that decreased with therapy but markedly increased with tumor persistence.42 This parameter may help distinguish patients with differing tumor responses, thus enabling clinicians to modify therapy. Further studies, however, are needed.
Ovary
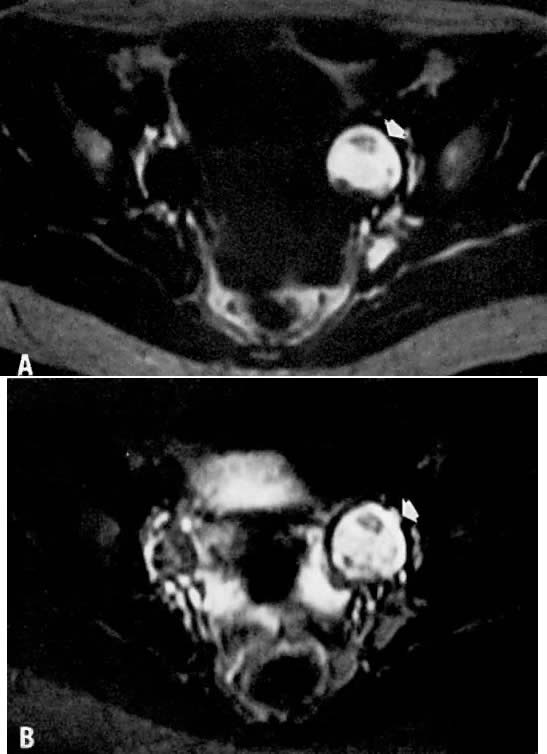
When an adnexal mass is found, it is often helpful to have a diagnosis of the lesion before an exploratory laparotomy is performed. Several types of ovarian lesions are particularly well evaluated by MRI; these include hemorrhagic cysts (Fig. 11), endometrial cysts, benign teratomas, and simple follicular cysts. MRI can readily identify hemorrhage because of relaxation differences between methemoglobin, fresh hemoglobin, and hemosiderin. However, depending on the biochemical state and age of the blood, the signal may be bright or dark on either T1- or T2-weighted images.43 Endometrial cysts tend to have more adhesions on the external surface and may lack a distinct margin from the uterine body.44 They may also demonstrate multiple loculations within the cyst. These loculations tend to have high-intensity signals on T1- and T2-weighted images, in contrast to water, which has high signal intensity on T2- and low signal intensity on T1-weighted images. In the fibrous tissue surrounding the cyst, a low-intensity area is occasionally identified surrounding areas of acute and chronic bleeding and is thought to represent the presence of hemosiderin-laden macrophages at the hematoma margin. One other feature that is characteristic of endometrial cysts is shading within loculi. Although the cause of the shading is not certain, it is thought to be due to the presence of deoxyhemoglobin in unlysed red blood cells or a higher concentration of paramagnetic (signal-enhancing) methemoglobin within those regions. The presence of any or all of these features should strongly suggest an endometrial cyst (Fig. 12). Further imaging using fat-saturation techniques significantly increases the diagnostic accuracy of MRI for endometriomas, particularly large-sized lesions.45 MRI has not been very sensitive in detecting endometrial implants.
Because of the large fat content within these tumors, ovarian cystic teratomas produce signal intensities very similar to that of adjacent fat on both T1- and T2-weighted images (Fig. 13). MRI may, in fact, be a more reliable diagnostic imaging modality for such lesions than ultrasonography. In a review of 23 surgically proven cases of ovarian teratomas in 18 patients, Togashi and colleagues noted that ultrasonography and radiography were able to demonstrate 19 of the 23 tumors and definitively identified only nine.46 Results of MRI, in contrast, were diagnostic in 20 of the 23 tumors, were highly suggestive in 2 other lesions, and were nonspecific in only 1 case. Definitive diagnosis could be made in lesions as small as 2 cm in diameter. In addition to the high signal intensity attributed to fat, debris and nodular protrusions are seen in these tumors. On occasion, teeth and bone are also identified as areas with negligible signals because of the high calcium and low water content, which yield little signal on proton imaging. Fat/fluid levels may occasionally be seen in teratomas. To distinguish fatty tumors from endometriomas, a unique pattern of chemical shift artifact, a boundary artifact also seen in fat, can be identified and used in conjunction with other characteristic findings.46
Simple, follicular, corpus luteum, mucinous, and serous cystadenomas may show similar MRI features. They tend to have low signal intensity on T1-weighted images and higher signal intensity on T2-weighted images. There are no differentiating signal characteristics between these cysts. As with ultrasonography, morphologic criteria may provide some specificity (Fig. 14).47, 48 Solid ovarian benign and malignant tumors tend to have variable T1 and T2 values and tend to have lower signal intensities overall. It is not currently possible to distinguish benign from malignant lesions based solely on the signal intensity. The diagnostic accuracy of MRI is reported to be only 60%, although it is more reliable than ultrasonography or CT.49 Image enhancement with gadolinium compound has reportedly increased characterization of malignant lesions from 56% to 78% while increasing staging accuracy from 63% to 75%.50 Such accuracy was possible with the use of previously established criteria, such as the size of the lesion, the presence of solid components and septations, the presence of a thickened cyst wall, and extraovarian involvement.
MRI has been used to study polycystic ovarian syndrome. It is particularly helpful in cases in which ultrasonographic examinations are equivocal. Because it provides superior resolution and tissue contrast, MRI has been able to assess ovarian morphology and has demonstrated subcapsular cysts and stromal hyperplasia not necessarily seen on sonograms because of limitations from ultrasound beam attenuation traveling through dense structures such as thickened ovarian capsules.51, 52
Vagina
Hricak and colleagues have shown that the vagina is easily identified by MRI (see Fig. 3). As in the uterus, the vaginal mucosa has high signal intensity on T2-weighted images, whereas the vaginal muscle itself has low signal intensity on both T1- and T2-weighted images.53 The muscle is clearly differentiated from the surrounding fat. The amount of vaginal mucus tends to fluctuate with the menstrual cycle. In 24 subjects, MRI was accurate in depicting the presence, partial absence, or total absence of the vagina. Identifying the presence of a vagina may be helpful in cases with suspected müllerian defects as well as in disorders of abnormal gonadal sex differentiations, such as Turner's syndrome.
Primary vaginal tumors are easy to identify, and their location, size, and extension into the vaginal wall can be distinguished.54 Tumors have medium signal intensity on T1-weighted images and tend to blend with adjacent vaginal tissue. Their appearance on T2-weighted scans is variable. When the tumor infiltrates the vaginal wall, the low signal intensity of the vaginal wall on T2-weighted images is distorted or no longer seen, and the tissue plane between the vagina and adjacent organs is obliterated. In one study, metastatic vaginal involvement separate from the known primary tumor was correctly identified in 21 of 22 patients.54 MRI detection of vaginal involvement was reported to be 92% accurate, 95% sensitive, and 90% specific. Again, however, the tumor intensity was found to be variable in this study. The overall role of MRI in vaginal carcinoma needs to be further defined, because the value of any imaging modality for assessing vaginal carcinoma has not yet been strongly supported.
Müllerian Anomalies
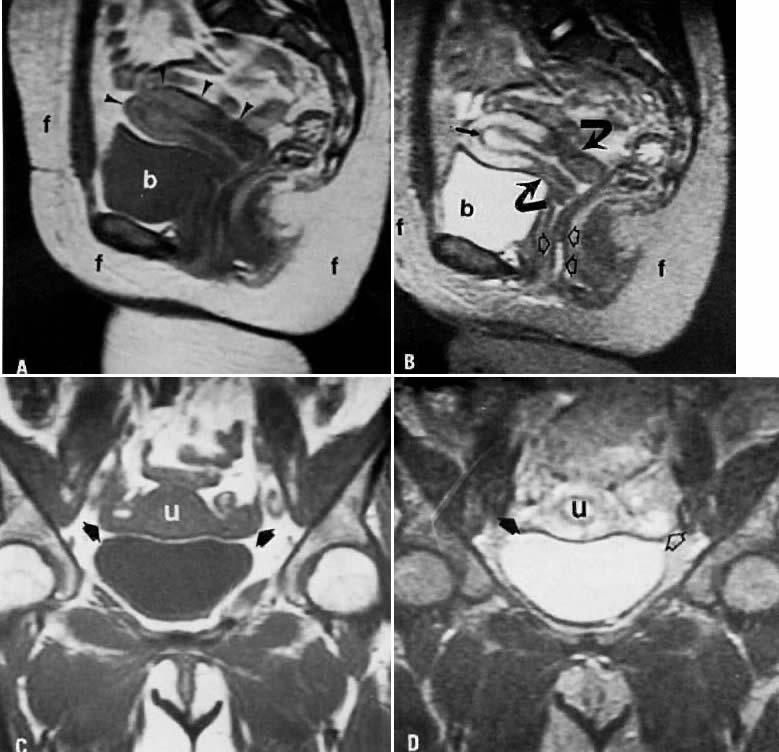
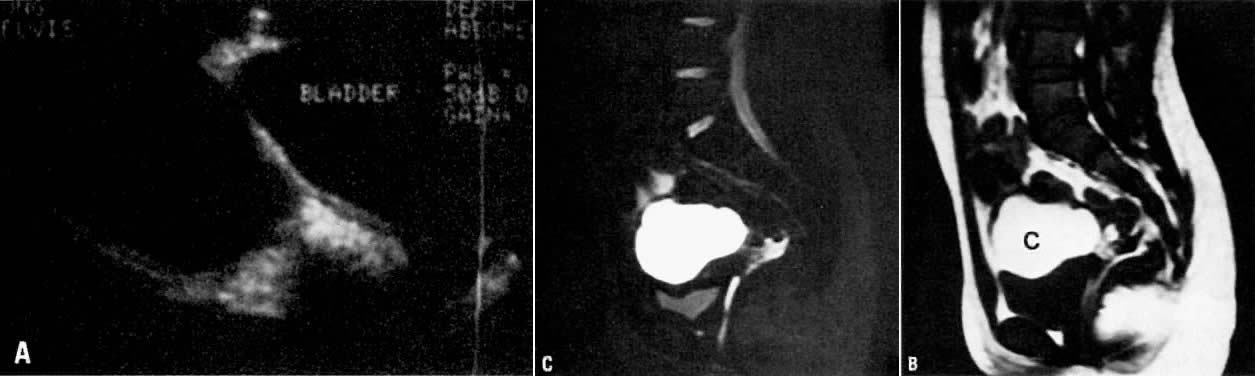
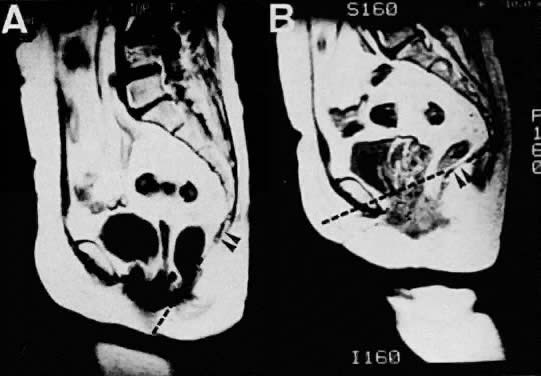
Although ultrasonography is a standard imaging modality in gynecology, there are several instances in which better definition of the internal female anatomy is necessary (e.g., in patients with müllerian anomalies). In a young adolescent patient, an informative, noninvasive imaging modality would be particularly valuable if it could replace diagnostic laparoscopy or laparotomy. Recent experience has demonstrated that MRI can be 100% accurate in müllerian duct anomalies55, 56 and appears to be superior to endovaginal ultrasonography and hysterosalpingography. Pubertal amenorrheic patients with cyclic lower abdominal pain should be evaluated for vaginal agenesis and the presence of a hematocolpos. MRI, with its multiplanar capabilities, has successfully demonstrated vaginal agenesis in the absence or presence of a cervix, uterus, and ovaries.57, 58, 59 In many cases, ultrasonography and CT imaging were performed in conjunction with MRI but proved limited in recognizing the endometrium, cervix, and vagina. MRI has been able to define the precise distance between the distal vaginal dimple and the upper patent vagina, thus facilitating preoperative planning of reconstructive surgery.
Because vaginal agenesis is often associated with a hematocolpos and sometimes with endometriosis, better definition of old and acute blood has been one advantage of MRI. The blood within the hematocolpos, as in endometriomas, may demonstrate variable signal intensity because of the presence of acute and chronic blood. Such differences would aid in the diagnosis of a pelvic mass in a young adolescent patient.
Uterine abnormalities such as a bicornuate uterus or a septate uterus have also been reported.60 Again, because of its multiplanar imaging capabilities, MRI has been able to identify the presence of more than one cervix. It has also been useful in tracing the extent of an intrauterine septum. These defects are often noted only at the time of surgery or at hysteroscopy.
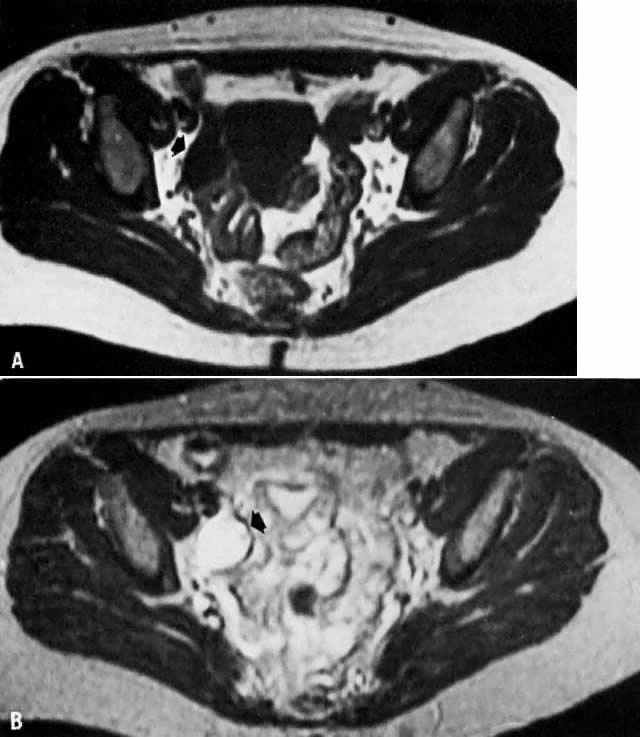
Nodal Assessment
One area where MRI has not proved to be very sensitive or specific is in the assessment of nodal tumor involvement. MRI has a tendency to miss tumor-positive lymph nodes.23 The accuracy of MRI in demonstrating lymph node involvement has been reported by Togashi and colleagues to be 84%.32 The sensitivity was 60%, and the specificity was 91%. Affected nodes tend to be brighter than muscle on T2-weighted images but darker than fat on T1-weighted images.61 Nodes less than 2 cm in diameter tend to yield more false-negative results.34 Although as accurate as CT scanning, MRI detection of pelvic lymphadenopathy is limited by longer imaging time, respiratory motion distortion, less optimal spatial resolution, and difficulty in differentiation from loops of bowel.62 At present, this form of nodal assessment cannot replace direct biopsy.
Pelvic Thrombosis
MRI has been shown to be useful in the diagnosis of deep venous thrombophlebitis of the lower extremities. In a recent study, the presence or absence of a deep venous thrombosis was correctly determined in 16 of 16 patients.63 MRI is exquisitely sensitive for detecting the presence of an intravascular clot and has a clear advantage over duplex Doppler ultrasonography because of its ability to study the internal deep venous system. Its use in puerperal pelvic thrombophlebitis, however, has not been clearly defined. Martin and colleagues were the first to use MRI to demonstrate an ovarian vein thrombosis in a postpartum patient,64 and Woo and associates demonstrated patent ovarian veins in 89% of puerperal patients.65 Further studies will, no doubt, demonstrate the utility of this sensitive and noninvasive tool in gynecologic patients.
Pelvic Floor Imaging
One area of great potential for the use of MRI is in the area of urogynecology. In the pelvic floor region, which is difficult to image by traditional methods, MRI has been able to demonstrate uterine prolapse and pelvic floor descent with standard and dynamic fast MR imaging. Sagittal images allow visualization of the levator plate, which loses its normal anatomic relationship to the symphysis pubis in the presence of uterine prolapse (Fig. 15).66 With the use of dynamic fast MR imaging and cinematic display, prolapse of the anterior, middle, and posterior compartments can be demonstrated during straining in patients with pelvic prolapse compared with normal patients.67 Such assessments may be valuable in preoperative planning and postoperative follow-up.
THE FUTURE OF MAGNETIC RESONANCE IMAGING IN GYNECOLOGY
It is obvious that one of the major uses for MRI in the future is for assessment of oncologic diseases, in terms of both staging and distinguishing benign processes such as fibrosis from recurrent disease. More studies need to be performed comparing current MRI with other imaging modalities on a blinded basis, and other techniques should be explored, such as multicoil, high-resolution, fast spin-echo MR imaging.4 We have no doubt that MRI will someday be the imaging technology of choice for many gynecologic diseases (Table 2).
TABLE 2. Utility of MRI in Gynecology Compared with Ultrasonography and CT
| MRI | Ultrasonography | CT |
Normal pelvic anatomy | + + + | + + + | + + + |
Leiomyomas | + + + | + + | + + |
Adenomyosis | + + | - | ? |
Endometrial cancer | + + | - | + |
Myometrial invasion | + + + | - | + / - |
Cervical cancer | + + + | - | + + |
Vaginal cancer | + + | - | + |
Ovarian cysts |
|
|
|
Simple/functional | + + | + + + | + |
Hemorrhagic | + + | + | + |
Dermoid | + + + | + + | + |
Endometrioma | + | - | - |
Ovarian cancer | + / - | + / - | + |
Müllerian anomalies | + + | + + | ? |
Tumor involvement of | + / - | - | + /- |
pelvic nodes |
|
|
|
Pelvic thrombophlebitis | + + | + | + |
Future innovations that may have significant clinical impact include the development and use of contrast agents that should allow further tissue differentiation. Also exciting are the prospects for performing in vivo tissue spectroscopy, a biochemical means for studying the presence of specific molecules. Spectra from tumors are demonstrably different from those of normal tissue.68 It has been suggested that spectroscopy may enable more accurate monitoring of tumor response to therapy than is shown by currently available tests. Finally, ongoing research into imaging with other nuclei such as 13C and 31P will yield more insights into the biochemical behavior of both normal and pathologic tissue.
REFERENCES
Hennig J, Nauerth A, Friedburg H: RARE imaging: A fast imaging method for clinical MR. Magn Reson Med 3: 823, 1986 |
|
Listerud J, Einstein S, Outwater E, Kressel HY: First principles of fast spin echo. Magn Reson Q 8: 199, 1992 |
|
Smith RC, Reinhold C, Lange RC et al: Fast spin echo MR imaging of the female pelvis: Part I. Use of a whole volume coil. Radiology 184: 665, 1992a |
|
Smith RC, Reinhold C, McCauley TR et al: Multicoil high resolution fast spin echo MR imaging of the female pelvis. Radiology 184: 671, 1992b |
|
Budinger TF: Biological and environment hazards. In Higgins CB, Hricak H (eds): Magnetic Resonance Imaging of the Body, pp 539–545. New York, Raven Press, 1987 |
|
Spritzer CE, Kressel HY, Mitchell D: Magnetic resonance imaging of the female pelvis. In Kressel HY (ed): Magnetic Resonance Annual, pp 203–235. New York, Raven Press, 1987 |
|
McCarthy S, Scott G, Majumdar S et al: Uterine junctional zone: MR study of water content and relaxation properties. Radiology 171: 241, 1989 |
|
Hricak H: MRI of the female pelvis: A review. AJR 146: 1115, 1986 |
|
McCarthy S: Magnetic resonance imaging in the evaluation of infertile women. Magn Reson Q 6: 239, 1990 |
|
McCarthy S, Vaquero E: Gynecologic anatomy with magnetic resonance imaging. Am J Obstet Gynecol 155: 255, 1986 |
|
Stark DD, McCarthy SM, Filly RA et al: Pelvimetry by magnetic resonance imaging. AJR 144: 947, 1985 |
|
Demas BE, Hricak H, Jaffe RB: Uterine MR imaging: Effects of hormonal stimulation. Radiology 159: 123, 1986 |
|
Hamlin DJ, Pettersson H, Fitzsimmons J, Morgan LS: MR imaging of uterine leiomyomas and their complications. J Comput Assist Tomogr 9: 902, 1985 |
|
Hricak H, Tscholakoff D, Heinrichs L et al: Uterine leiomyomas: Correlation of MR, histopathologic findings, and symptoms. Radiology 158: 385, 1986 |
|
Dudiak CM, Turner DA, Patel SK et al: Uterine leiomyomas in the infertile patient: Preoperative localization with MR imaging versus US and hysterosalpingography. Radiology 167: 627, 1988 |
|
Lee JKT, Gersell DJ, Balfe DM et al: The uterus: In vitro MR-anatomic correlation of normal and abnormal specimens. Radiology 157: 175, 1985 |
|
Shapeero LG, Hricak H: Mixed mu¨llerian sarcoma of the uterus: MR imaging findings. AJR 153: 317, 1989 |
|
Worthington JL, Balfe DM, Lee JKT et al: Uterine neoplasms: MR imaging. Radiology 159: 725, 1986 |
|
Togashi K, Nishimura K, Itoh K et al: Adenomyosis: Diagnosis with MR imaging. Radiology 166: 111, 1988 |
|
Mark AS, Hricak H, Heinrichs LW et al: Adenomyosis and leiomyoma: Differential diagnosis with MR imaging. Radiology 163: 527, 1987 |
|
Togashi K, Ozasa H, Konishi I et al: Enlarged uterus: Differentiation between adenomyosis and leiomyoma with MR imaging. Radiology 171: 531, 1989 |
|
McCarthy S, Tauber C, Gore J: Female pelvic anatomy: MR assessment of variations during the menstrual cycle and with use of oral contraceptives. Radiology 160: 119, 1986 |
|
Powell MC, Womack C, Buckley J et al: Pre-operative magnetic resonance imaging of stage 1 endometrial adenocarcinoma. Br J Obstet Gynaecol 93: 353, 1986 |
|
Hricak H, Stern JL, Fisher MR et al: Endometrial carcinoma staging by MR imaging. Radiology 162: 297, 1987 |
|
Gordon AN, Fleischer AC, Dudley BS et al: Preoperative assessment of myometrial invasion of endometrial adenocarcinoma by sonography (US) and magnetic resonance imaging (MRI). Gynecol Oncol 34: 175, 1989 |
|
Belloni C, Vigano R, Del Maschio A et al: Magnetic resonance imaging in endometrial carcinoma staging. Gynecol Oncol 37: 172, 1990 |
|
Hirano Y, Kubo K, Hirai Y et al: Preliminary experience with gadolinium-enhanced dynamic MR imaging for uterine neoplasms. Radiographics 12: 243, 1992 |
|
Yamashita Y, Harada M, Sawada T et al: Normal uterus and FIGO stage I endometrial carcinoma: Dynamic gadolinium-enhanced MR imaging. Radiology 186: 495, 1993 |
|
Powell MC, Worthington BS, Sokal M et al: Magnetic resonance imaging-Its application to cervical carcinoma. Br J Obstet Gynaecol 93: 1276, 1986 |
|
Lien HH, Blomlie V, Iversen T et al: Clinical stage I carcinoma of the cervix. Acta Radiol 34: 130, 1993 |
|
Hricak H, Lacey CG, Sandles LG et al: Invasive cervical carcinoma: Comparison of MR imaging and surgical findings. Radiology 166: 623, 1988 |
|
Togashi K, Nishimura K, Sagoh T et al: Carcinoma of the cervix: Staging with MR imaging. Radiology 171: 245, 1989 |
|
Waggenspack GA, Amparo EG, Hannigan EV: MR imaging of uterine cervical carcinoma. J Comput Assist Tomogr 12: 409, 1988 |
|
Janus CL, Mendelson DS, Moore S et al: Staging of cervical carcinoma: Accuracy of magnetic resonance imaging and computed tomography. Clin Imaging 13: 114, 1989 |
|
Fishman Javitt MC, Stein HL, Lovecchio JL: MRI in staging of endometrial and cervical carcinoma. Magn Reson Imaging 5: 83, 1987 |
|
Burghardt E, Hofmann HMH, Ebner F et al: Magnetic resonance imaging in cervical cancer: A basis for objective classification. Gynecol Oncol 33: 61, 1989 |
|
Rubens D, Thornbury JR, Angel C et al: Stage IB cervical carcinoma: Comparison of clinical, MR, and pathologic staging. AJR 150: 135, 1988 |
|
Ebner F, Kressel HY, Mintz MC et al: Tumor recurrence versus fibrosis in the female pelvis: Differentiation with MR imaging at 1.5 T. Radiology 166: 333, 1988 |
|
Williams MP, Husband JE, Heron CW et al: Magnetic resonance imaging in recurrent carcinoma of the cervix. Br J Radiol 62: 544, 1989 |
|
Hricak H, Swift PS, Campos Z et al: Irradiation of the cervix uteri: Value of unenhanced and contrast-enhanced MR imaging. Radiology 189: 381, 1993 |
|
Hawnaur JM, Johnson RJ, Hunter RD et al: The value of magnetic resonance imaging in assessment of carcinoma of the cervix and its response to radiotherapy. Clin Oncol 4: 11, 1992 |
|
Santoni R, Bucciolini M, Chiostrini MD et al: Quantitative magnetic resonance imaging in cervical carcinoma: A report on 30 cases. Br J Radiol 64: 498, 1991 |
|
Hamlin DJ, Fitzsimmons JR, Pettersson H et al: Magnetic resonance imaging of the pelvis: Evaluation of ovarian masses at 0.15 T. AJR 145: 585, 1985 |
|
Nishimura K, Togashi K, Itoh K et al: Endometrial cysts of the ovary: MR imaging. Radiology 162: 315, 1987 |
|
Sugimura K, Okizuka H, Imaoka I et al: Pelvic endometriosis: Detection and diagnosis with chemical shift MR imaging. Radiology 188: 435, 1993 |
|
Togashi K, Nishimura K, Itoh K et al: Ovarian cystic teratomas: MR imaging. Radiology 162: 669, 1987 |
|
Mawhinney RR, Powell MC, Worthington BS, Symonds EM: Magnetic resonance imaging of benign ovarian masses. Br J Radiol 61: 179, 1988 |
|
Dooms GC, Hricak H, Tscholakoff D: Adnexal structures: MR imaging. Radiology 158: 639, 1986 |
|
Smith FW, Cherryman GR, Bayliss AP et al: A comparative study of the accuracy of ultrasound imaging, x-ray computerized tomography and low field MRI diagnosis of ovarian malignancy. Magn Reson Imaging 6: 225, 1988 |
|
Stevens SK, Hricak H, Stern JL: Ovarian lesions: Detection and characterization with gadolinium-enhanced MR imaging at 1.5 T. Radiology 181: 481, 1991 |
|
Faure N, Prat X, Bastide A, Lemay A: Assessment of ovaries by magnetic resonance imaging in patients presenting with polycystic ovarian syndrome. Hum Reprod 4: 468, 1989 |
|
Mitchell DG, Gefter WB, Spritzer CE et al: Polycystic ovaries: MR imaging. Radiology 160: 425, 1986 |
|
Hricak H, Chang YCF, Thurnher S: Vagina: Evaluation with MR Imaging. I. Normal anatomy and congenital anomalies. Radiology 169: 169, 1988 |
|
Chang YCF, Hricak H, Thurnher S, Lacey CJ: Vagina: Evaluation with MR Imaging. II. Neoplasms. Radiology 169: 175, 1988 |
|
Carrington BM, Hricak H, Nuruddin RN et al: Mu¨llerian duct anomalies: MR imaging evaluation. Radiology 176: 715, 1990 |
|
Pellerito JS, McCarthy SM, Doyle MB et al: Diagnosis of uterine anomalies: Relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 183: 795, 1992 |
|
Togashi K, Nishimura K, Itoh K et al: Vaginal agenesis: Classification by MR imaging. Radiology 162: 675, 1987 |
|
Vainright JR, Fulp CJ, Schiebler ML: MR imaging of vaginal agenesis with hematocolpos. J Comput Assist Tomogr 12: 891, 1988 |
|
Barach B, Falces E, Benzian SR: Magnetic resonance imaging for diagnosis and preoperative planning in agenesis of the distal vagina. Ann Plast Surg 19: 192, 1987 |
|
Hamlin DJ, Pettersson H, Ramey SL, Moazam F: Magnetic resonance imaging of bicornuate uterus with unilateral hematometrosalpinx and ipsilateral renal agenesis. Urol Radiol 8: 52, 1986 |
|
Dooms GC, Hricak H, Crooks LE, Higgins CB: Magnetic resonance imaging of the lymph nodes: Comparison with CT. Radiology 153: 719, 1984 |
|
Lee JKT, Heiken JP, Ling D et al: Magnetic resonance imaging of abdominal and pelvic lymphadenopathy. Radiology 153: 181, 1984 |
|
Spritzer CE, Sussman SK, Blinder RA et al: Deep venous thrombosis evaluation with limited-flip-angle, gradient-refocused MR imaging: Preliminary experience. Radiology 166: 371, 1988 |
|
Martin B, Mulopulos GP, Bryan PJ: MRI of puerperal ovarian-vein thrombosis (case report). AJR 147: 291, 1986 |
|
Woo GM, Twickler DM, Stettler RW et al: The pelvis after cesarean section and vaginal delivery: Normal MR findings. AJR 161: 1249, 1993 |
|
Ozasa H, Mori T, Togashi K: Study of uterine prolapse by magnetic resonance imaging: Topographical changes involving the levator ani muscle and the vagina. Gynecol Obstet Invest 34: 43, 1992 |
|
Yang A, Mostwin JL, Rosenshein NB, Zerhouni EA: Pelvic floor descent in women: Dynamic evaluation with fast MR imaging and cinematic display. Radiology 179: 25, 1991 |
|
Radda G: The use of NMR spectroscopy for the understanding of disease. Science 233: 640, 1986 |